GET BETTER FASTER!!
Welcome to Kinetic Relief, where our passion for health and commitment to holistic well-being converge. We are a top provider of non-invasive treatments for soft-tissue and nerve problems, including strains, sprains, and musculoskeletal disorders.
Our hands-on, movement-focused method quickly relieves pain and restores function, offering a faster and more complete recovery than conventional therapy methods.
Committed to Your Health and Wellness Journey
Recognizing that each person is unique, we prioritize a patient-centered approach. From the moment you walk through our doors, our goal is to understand your individual needs, concerns, and goals —we are partners in your journey towards optimal health.
Our clinicians are currently some of the only Active Release Techniques certified practitioners in the area. For information about the Active Release Technique, please visit www.activerelease.com.
The fastest way to schedule an appointment is to click the "Book Appointment" link below. However, if you are unable to find an available appointment online, please call or text (817) 730-5995!
30 +
Years of Combined Experience
8 +
Techniques & Modalities
Our Vision
We envision a world where individuals are empowered to take control of their health.
Our Mission
We aim to be a trusted partner in our patients' pursuit of a vibrant and pain-free life.
Committed to Your Health and Wellness Journey
Recognizing that each person is unique, we prioritize a patient-centered approach. From the moment you walk through our doors, our goal is to understand your individual needs, concerns, and goals —we are partners in your journey towards optimal health.
Our clinicians are currently some of the only Active Release Techniques certified practitioners in the area. For information about the Active Release Technique, please visit www.activerelease.com.
The fastest way to schedule an appointment is to click the "Book Appointment" link below. However, if you are unable to find an available appointment online, please call or text (817) 730-5995!
30 +
Years of Experience
8 +
Techniques & Modalities
Our Vision
We envision a world where individuals are empowered to take control of their health,
Our Mission
We aim to be a trusted partner in our patients' pursuit of a vibrant and pain-free life.
Our Services & What We Treat
Non-invasive pain relief
Corrective Exercise
Consulting
Back Pain
Carpal Tunnel Syndrome
Chronic Pain
Foot and Ankle Injuries
Life Coaching
Muscle Tension and Joint Pain
Neck Pain
Physical Wellness
Shoulder Conditions
Spine Conditions
Sport Injuries
Trauma
Our Services & What We Treat
Non-invasive Pain Relief
Corrective Exercise
Consulting
Back Pain Relief
Carpal Tunnel Syndrome
Chronic Pain
Foot and Ankle Injuries
Life Coaching
Muscle Tension and Joint Pain
Neck Pain
Physical Wellness
Shoulder Condition
Spine Conditions
Sport Injuries
Trauma
1,000 +
Happy Patients
30+ yrs
Combined Experience
Multiple
Techniques & Modalities
2
Locations
Our Clinicians
M. Chad Gann, PhD is an experienced Athletic Trainer (AT), Registered Nurse (RN), and Licensed Paramedic (LP) with extensive experience treating musculoskeletal dysfunction. Chad is passionate about utilizing non-invasive and non-pharmacological techniques to treat pain and discomfort. Additionally, he is a committed educator and healthcare professional with a diverse background and experience in sports medicine, performance psychology, emergency response, and whole-person healthcare. Based in Burleson, Texas, Chad is the Founder and CEO of Kinetic Relief (Integrative Wellness & Rehabilitation, PLLC). With over two decades of experience, he has held roles as a 911 paramedic, emergency room nurse, mental health nursing professor, and police officer. Chad's law enforcement experience includes patrol operations, homeland security and special events, and Special Weapons and Tactics (SWAT). Currently, Chad is completing a Doctor of Philosophy degree in Health Science from Liberty University School of Health Sciences. His specialty certifications include Active Release Technique (ART), Dry Needling (MDNc), Corrective Exercise (CES), and Performance Enhancement (PES).
M. Chad Gann, PhD, BSN, LAT, ATC, RN, LP
Treatment Location: By Appointment
Ben Hooper is a dedicated Athletic Trainer and Corrective Exercise Specialist in the Grapevine-Colleyville School District. He has extensive training and experience treating musculoskeletal dysfunction having served as a clinical Athletic Trainer at The Orthopedic and Sports Medicine Institute (served as surgical first-assist for Dr. Todd Moore), as Head Athletic Trainer at Ennis ISD and additional service at Kennedale and Jacksonville ISDs. He holds a Master of Science in Athletic Training from Stephen F. Austin State University and a Bachelor of Science in Kinesiology from Howard Payne University. Ben is certified as an athletic trainer, orthopedic technician, corrective exercise specialist, and x-ray technician. He enjoys camping, sports, and family time, and is a passionate Green Bay Packers fan. Ben's specialty certifications include Active Release Technique (ART) and Corrective Exercise (CES).
Ben Hooper, MS, LAT, ATC, OTC, ART, CES
Treatment Location: Innately Chiropractic, Grapevine, TX
GENERAL FAQS
What is an Athletic Trainer?
Athletic trainers (ATs) are highly qualified, multi-skilled health care professionals who render service or treatment, under the direction of or in collaboration with a physician, in accordance with their education, training and the state's statutes, rules and regulations. As a part of the health care team, services provided by athletic trainers include primary care, injury and illness prevention, wellness promotion and education, emergent care, examination and clinical diagnosis, therapeutic intervention and rehabilitation of injuries and medical conditions. The National Athletic Trainers' Association (NATA) Code of Ethics states the principles of ethical behavior that should be followed in the practice of athletic training (National Athletic Trainers' Association, 2021).
Athletic trainers are sometimes confused with personal trainers. However, there is a significant difference in the education, skillset, job duties, and patients of an athletic trainer when compared with a personal trainer. The athletic training academic curriculum and clinical training follows the medical model. Athletic trainers must graduate from an accredited baccalaureate or master’s program, and 70% of ATs have a master’s degree (National Athletic Trainers' Association, 2021).
What is required to become a Certified Athletic Trainer (ATC)/Licensed Athletic Trainer (LAT)?
To become a athletic Trainer, a student must graduate with bachelors or master’s degree from an accredited professional athletic training education program and pass a comprehensive test administered by the Board of Certification (BOC). Once certified, he or she must meet ongoing continuing education requirements in order to remain certified. (National Athletic Trainers' Association)
What are the major training and education practice domains for Athletic Trainers?
BOC-certified athletic trainers are educated, trained and evaluated in five major practice domains including injury and illness prevention and wellness promotion, examination, assessment and diagnosis, immediate and emergency care, therapeutic intervention, health care administration, and professional responsibility (National Athletic Trainers' Association, 2021).
Where do most athletic trainers work and who can they treat?
Athletic trainers treat a wide range of patients and can work in a variety of settings. Regardless of their practice setting, athletic trainers practice according to their education, scope of practice, and state practice act. Athletic trainers work in public and private secondary schools, colleges and universities, professional and Olympic sports, youth leagues, municipal and independently owned youth sports facilities, physician practices (similar to nurses, physician assistants, physical therapists and other professional clinical personnel), rural and urban hospitals, hospital emergency rooms, urgent and ambulatory care centers, clinics with specialties in sports medicine, cardiac rehab, medical fitness, wellness and physical therapy, occupational health departments in commercial settings (including manufacturing, distribution and offices to assist with ergonomics), police and fire departments and academies, municipal departments, branches of the military, and performing arts (including professional and collegiate level dance and music). (National Athletic Trainers' Association)
Does Kinetic Relief have a Medical Director?
Yes, our Medical Director is G. Todd Moore, DO, a board certified and fellowship trained sports medicine and orthopedic surgeon specializing in all aspects of orthopedics with special interests in hip and knee arthroplasty, fracture care, and pediatric orthopedics. Dr. Moore has been in practice in the DFW area since 2012. His principle practice is a part of The Orthopedic and Sports Medicine Institute in Mansfield.

Active Release Technique FAQS
How long does active release technique take to work?
Here's what patients can expect from ART therapy: Treatment frequency – Varies by degree and duration of injury. During treatment – Procedures don't cause pain, though discomfort may be caused due to manipulation of sore tissue. Results – Improvement felt within between one to six visits, depending on injury severity.
Does active release technique really work?
ART is an effective treatment for a variety of conditions and injuries of the soft tissues, such as overuse and sports injuries. It can help relieve pain and stiffness and help restore your range of motion so you can return to your favorite activities.
What are the principles of active release technique?
Active Release Technique (ART) is a type of myofascial release technique. This treatment method involves manual (hands-on) soft tissue therapy and movement. The aim is to break up scar tissue to promote healing. It may lessen pain and restore range of motion for people with acute or chronic injuries
Is active release technique the same as chiropractic?
Active Release Technique, or A.R.T., for short, is a type of Chiropractic treatment that focuses on treating the soft-tissue system of the body. And unlike traditional Chiropractic treatment, it uses massage-like movements rather than adjustments.
Is Active Release Technique the same as myofascial release?
Myofascial release is a way of manipulating and restoring movement to tissues that surround your muscles called fascia. Active Release Technique (ART) is arguably the most advanced and effective form of myofascial release ever created.
What are the benefits of active release therapy?
The benefits of ART include a decrease of pain in the affected area and an increase in mobility and strength. By breaking down scar tissue, active release can improve your circulation and range of motion, helping you move more easily.
Graston Technique® FAQS
What conditions can be treated with the Graston Technique®?
GT-trained clinicians use GT instruments to effectively and efficiently address soft tissue lesions and fascial restrictions while treating acute and chronic conditions, including: Achilles Tendinitis/osis (ankle pain) Carpal Tunnel Syndrome (wrist pain) Cervicothoracic Sprain/Strain (neck pain) Fibromyalgia Lateral Epicondylitis/osis (tennis elbow) Lumbosacral Sprain/Strain (back pain) Medial Epicondylitis/osis (golfer’s elbow) Myofascial Pain Syndromes Patellofemoral Disorders (knee pain) Plantar Fasciitis/osis (foot pain) Post surgeries such as joint replacements, RTC repairs (once post-surgical protocol allows for soft tissue mobilization/manual therapy) Rotator Cuff Tendinitis/osis (shoulder pain) Scar Tissue/post-surgical scars (once completely closed) Patients demonstrating central and/or peripheral sensitization (only used in light stroking/brushing mode to desensitize) Shin Splints Trigger Finger Women’s Health (post-mastectomy and Caesarean scarring) Graston Technique® can be used to treat any movement system dysfunction that has been determined to have a soft tissue component.
Is Graston Technique® an Evidenced-Based Form of Manual Therapy?
Empirical and anecdotal evidence exists for the following physiological effects of GT: Separates and breaks down collagen cross-links, and splays and stretches connective tissue and muscle fibers Facilitates reflex changes in the chronic muscle holding pattern (inhibition of abnormal tone/guarding leading to pain reduction via improved sensory input) Alters/inhibits spinal reflex activity (facilitated segment) Increases the rate and amount of blood flow to and from the area (angiogenesis vs. immediate local increases in blood flow) Increases cellular activity in the region, including fibroblasts and mast cells Increases histamine response secondary to mast cell activity
How is scar tissue different from other tissue?
When viewed under a microscope, normal tissue can be organized in a couple of different fashions: dense, regular elongated fibers running in the same direction, such as tendons and ligaments; or dense and loose, irregular with fibers running in multiple directions. In either instance, when tissue is damaged, it will often heal in a fibrotic, haphazard manner and may appear radio-dense under diagnostic ultrasound. The tissue may show thickening, irregular organization or less precise margins as compared to non-injured tissues, which results in a restricted range of motion and, very often, pain and functional limitations.
Why is scar tissue a problem?
Scar tissue limits range of motion due its negative impact on sensory motor firing rates and frequencies. Abnormal sensory inputs perpetuate a dysfunctional cycle of nervous system sensitization, pain and dysfunctional movement/motor output. GT offers a positive method of manual therapy that interrupts and breaks this cycle of pain and dysfunctional movement.
Will GT treatments affect my everyday activities?
Patients that have progressed beyond the acute stages of inflammation and repair are often encouraged to resume a pain-free level of activity and exercise with the modifications that are determined by their GT-trained health professional. GT is designed to be implemented with appropriate therapeutic exercises and activities to achieve an ideal outcome.
What kind of results does Graston Technique® produce?
Historically, the Graston Technique® has had positive outcomes in 75-90 percent of all conditions treated. It is equally effective in restoring function to acute and chronic injuries, pre- and post-surgical patients and maintaining optimal range of motion.
Is Graston Technique® something new?
The concept of cross fiber massage is not new. Graston Technique® is grounded in the works of Dr. James Cyriax, a British orthopedic surgeon.
Dry Needling FAQS
What is dry needling?
Dry needling uses a fine monofilament, sterile needle to treat tender muscles (trigger points), neuro-muscular pain, or movement dysfunctions. The therapy is NOT acupuncture and is based completely on a Western medical model. Dry needling requires thorough examination and diagnosis by your physical therapist in order and treats dysfunctions specific to you as an individual
How does this therapy help me?
The benefits can include
● decrease in muscle tightness,
● pain, or
● dysfunction due to chronic or acute musculoskeletal conditions.
Does dry needling hurt?
Dry needling uses very thin needles which, typically, are not painful. Occasionally, a patient feels a small pinprick. Because the needles do not contain medication, we use very thin needles that are 8x smaller than those used for your vaccines. While some areas may be more tender than others, dry needling typically does not cause more pain than your current symptoms.
How long does a session last? In general, how many treatments will I need?
A typical dry needling session usually lasts 10-15 minutes. Additionally, when indicated, your therapist may utilize electrical intramuscular stimulation to elicit twitch responses in multiple muscles in order to decrease pain. In acute pain situations, only one session may be needed. For more chronic pain situations, it may take several treatments to notice a change. Because dry needling can have a cumulative effect, if you do not notice results after the first session, we typically recommend 2-3 treatments before deciding to pursue other options.
What should I do after a treatment?
After a treatment, you may do the following based on your comfort level. Please note that if it hurts or exacerbates your symptoms, then discontinuing the activity is best.
● Work out and/or stretch
● Participate in normal physical activity
● Massage the area
● Use heat or ice as preferred for post treatment soreness
● If you have prescription medications, continue to take them as prescribed
What should I not do after the needling therapy?
● Unfamiliar physical activities or sports
● Doing more than you normally do
● Excessive alcohol intake
How deep do needles go?
Typically 0.5 inches to 4 inches, the needles used depend on the muscle tissue being treated. For example, the therapist can use a 1 inch needle to treat the upper trapezius when a 4 inch needle gets used to access deeper muscles such as the piriformis in the hip. Longer needles are not associated with more pain.
What type of risks are associated with myofascial trigger point dry needling?
The most serious risk associated with dry needling is pneumothorax (air in the space around the lungs). This is a very rare (<.01%) but serious complication and would require the patient to seek medical attention. Symptoms of pneumothorax include shortness of breath, sudden sharp pain each time you breath in, and inability to “catch your breath.” Other risks include bruising (7.55%), bleeding (4.65%), pain (.088%), headache (0.14%), nausea (0.13%), infection (<.1%).
Who performs the treatment on me? What are their qualifications?
The therapy is usually performed by a physical therapist. Not all therapists, however, can offer their clients dry needling. In most states, a practitioner must have a certain amount of education and training in the therapy before being certified to treat patients.
How many needles are used?
On average, 5-10 needles may be used to effectively treat the involved muscles. Occasionally, larger muscle groups may require the use of more needles.
Does this therapy loosen muscles or relax muscle knots?
Yes, needling can be used in tight muscles/knots in order to elicit a twitch response or muscle cramp prior to causing the muscle to relax.
Does Medicare pay for dry needling?
At this time, Medicare does not cover this therapy. In 2020, CMS proposed a final rule to add CPT codes for the therapy, however Medicare will not reimburse for these codes due to lack of studies conducted to support the use of needling. Expect change as the evidence supporting dry needling sharply increases. Some commercial insurances cover this treatment, but you may have to contact your individual insurance in order to determine coverage.
Does this release toxins?
Dry needling activates the body to release opiate peptides like beta-endorphins, enkephalins, and dynorphins. These are natural neurotransmitters that work to block transmission of pain information to the brain and spinal cord.
Are there any infection risks?
The risk of infection is extremely low (<0.1%).
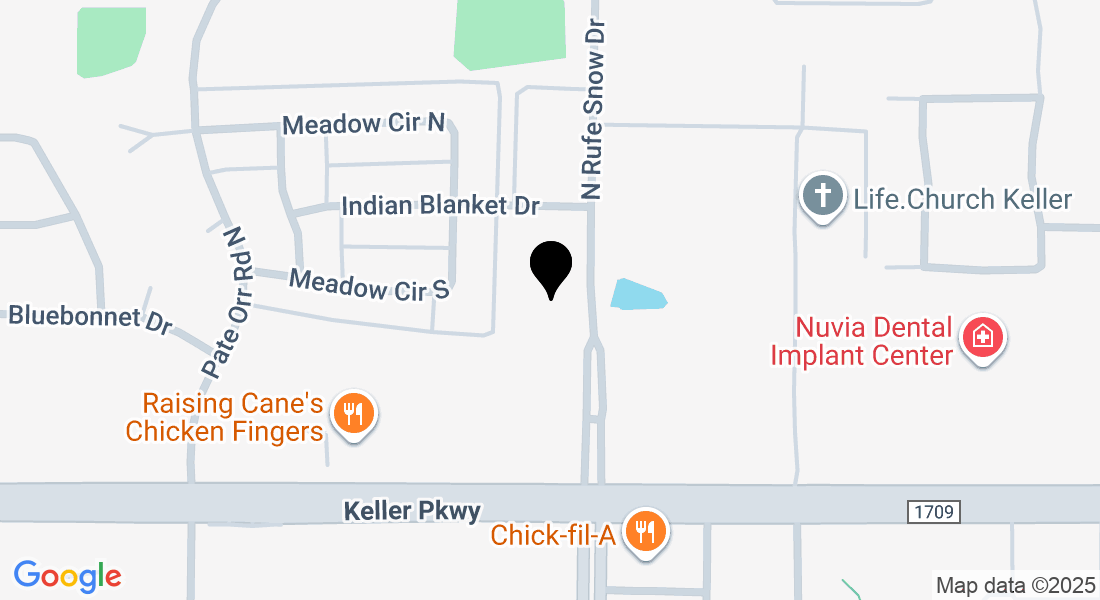
Treatment Locations
KINETIC RELIEF
Innately Chiropractic
Get In Touch
Call / Text: 817-730-5995
Email: [email protected]
Get In Touch
Call / Text: 817-730-5995
Email: [email protected]